“Articulate, intelligent individuals can skillfully construct a convincing case to argue almost any point of view. This critical, reactive use of intelligence narrows our vision. In contrast, projective thinking is expansive, ‘open-ended’ and speculative, requiring the thinker to create the context, concepts, and the objectives” — Linda Stone. Feb 6, 2011.
I couldn’t agree with Linda Stone more on this matter. I would only add that in the clinical technology world we apply a lot of historical perspective to dig into our philosophical foxholes. We often make the mistake of failing to carefully observe the new trends and requirements in our industry and step towards necessary changes to address these objectives. While our hard-earned lessons can be a great platform for continual success, they can also be a millstone around our neck if we don’t know how to let go when necessary.
I’m sure all of us in healthcare technology leadership positions want to be ready for all the changes headed our way, but I would be a liar if I didn’t admit that I have seen many of us looking backwards more than forward. When I struggle to leave my traditional point of view, I often find myself analyzing the potential pitfalls of such a move by looking back on what worked for me in the past. The following concept is in no way original. Just do a web search on “suspending disbelief” and you may be amazed at what you will find. When I was writing a reflection for a meeting a few years ago, I wanted to write something that would get my team to consider a very important idea:
“Consider that there’s a possibility that we should be changing everything we are currently doing.”
I stumbled upon Linda Stone while doing that research. The term “suspending disbelief” sounded odd at first. It’s a more elegant way to say “stop not believing,” which doesn’t sound very intellectual. But in fact, it is very practical. When I’ve wanted to move my team to a new place mentally, I’ve had to fight against the fact that where they are now was also established by an intellectual process.
We have developed procedures based on our beliefs and goals at the time. I have worked with many biomed programs over the years. They all are very similar, and that’s because we all have the same basic mission; repair and maintenance of medical equipment. We have worked with the same regulatory requirements for many years, so our methods conformed to that environment. With that said, I truly believe we are looking at a future that is markedly different than what we have experienced in the past 20 years.
I see sweeping changes in the way we do preventive maintenance, driven by the new CMS regulations. The AEM program directives have been a huge concern for our group. I have three talented young leaders working hard to build our program to address all those concerns in a way that honors our lean workforce directives. You may have had a chance to hear them speak at one of our industry conferences.
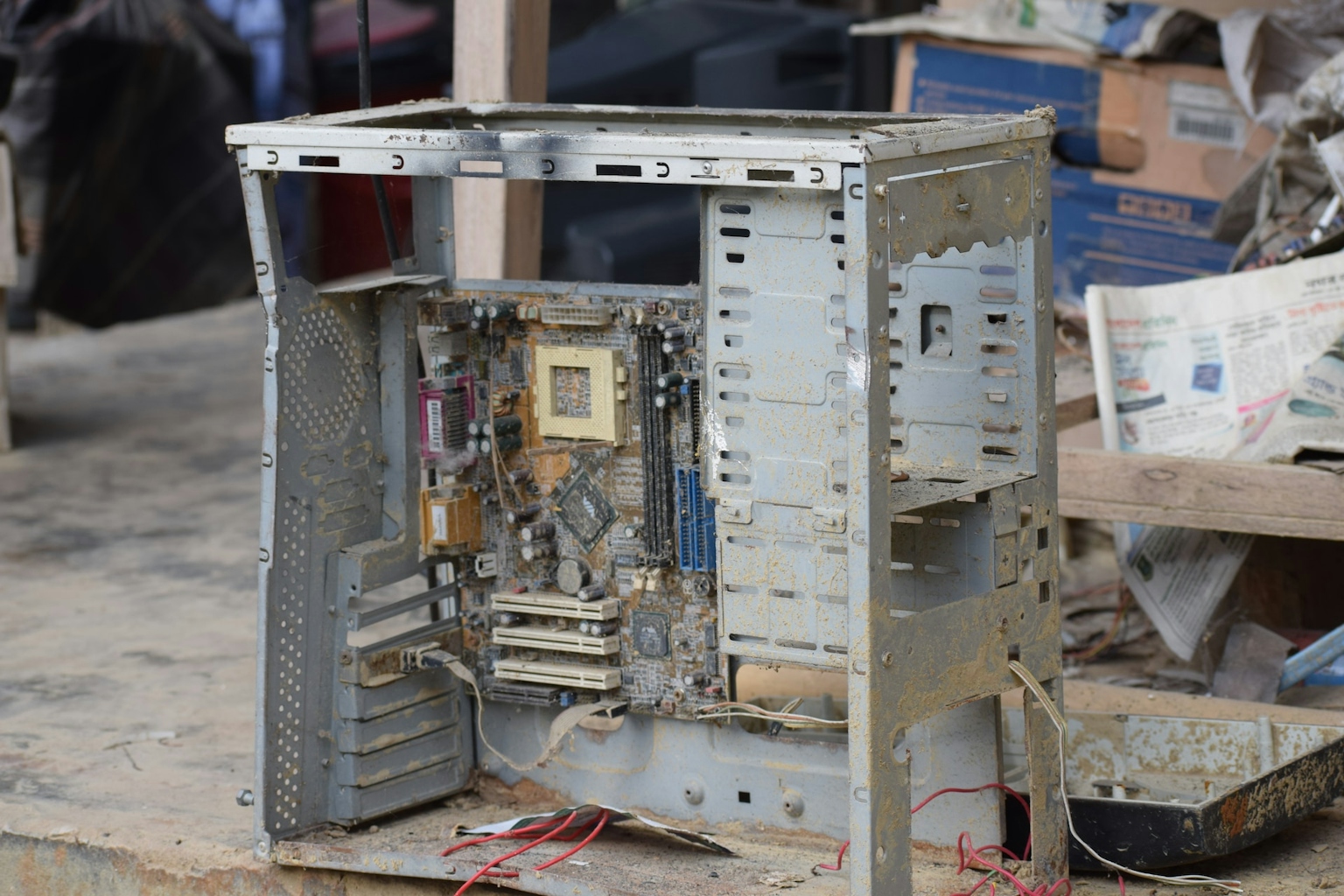
I also see an environment where capital dollars are going to be very sparse. We will be forced to view the whole replacement process in a different way. We might have to stop believing that an end-of-life notification from the manufacturer is the absolute trigger for capital replacement. We will likely be extending the life of many items well past the EOL notifications. ISO parts providers will be in greater demand. Scavenging from de-installed systems will be more common.
Some of you might find this idea very distasteful; some are already experts in this practice. Less common, but more disturbing, is the belief that high-end imaging equipment can’t be effectively serviced by “in-house” or non-OEM service people. I have worked with institutions ranging from small rural hospitals to large academic medical centers, which have all their imaging equipment on full service agreements with the manufacturers.
During my post analysis debriefings, I have had directors of radiology stare at me in absolute disbelief when I recommend training their current technicians and transferring the service responsibilities for their X-ray rooms, cath labs, CTs, even MRIs to their in-house program. They just can’t believe it’s possible. The millions of dollars in savings, however, is a great motivator.
While it’s intimidating to be at odds philosophically with someone as important as the director of radiology, it’s really most disappointing when the director of the clinical technology program doesn’t believe his folks can do this work. Too often the clinical technology program is relegated to preventative maintenance and minor repairs. They are the ones who make phone calls when something breaks. I find this very sad because I know how great it is to work in a shop that does everything. The comradery that can develop in a full-service biomed shop is very satisfying for a technician.
Our industry is moving into a very challenging future. We will need to be agile if we are going to remain relevant and meet our new performance requirements. Why not sit down with your techs and brainstorm ways to do address the demands of your team? Give your technicians permission to suspend the beliefs that have shaped your services over the years. I am a great believer in shaping your future as opposed to letting it shape you.
George Hampton is the president of Tech Knowledge Associates, a clinical technology management provider that was formed to bring unique value to its clients by guaranteeing savings, capping their expenses and protecting them from catastrophic failures. For more information, contact TKA at info@ii-techknow.com or visit ii-techknow.com.